Go Upstream – Applying a Prevention Mindset to Workplace Mental Health
Jan 26, 2026This post was commissioned by the Arizona Chapter of the National Safety Council to promote it's upcoming Southwest Safety Conference 2026. It appears at Guest Post: Go Upstream - Applying a Prevention Mindset to Workplace Mental Health - National Safety Council - Arizona Chapter.
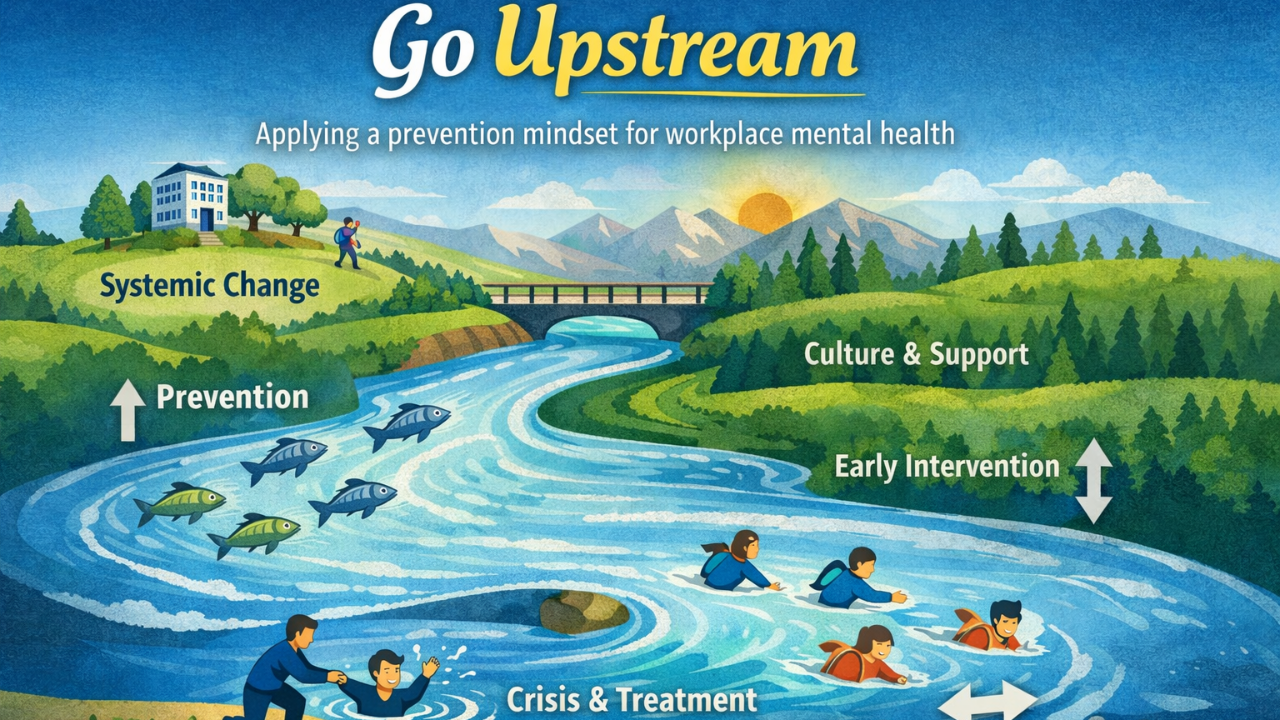
When dead fish begin appearing downstream, no one solves the problem by standing on the riverbank counting them. We go upstream to find the source of pollution. The fish are the outcome—not the cause.
Safety professionals understand this instinctively. When injuries, incidents, or near misses occur, you do not wait for the next serious event to confirm there is a problem. You investigate conditions, behaviors, and systems upstream and act early to prevent harm.
When it comes to employee mental health, however, many organizations are still standing downstream responding to crisis, burnout, or tragedy after the fact. I have seen this firsthand, and, sadly, then it is too late to intervene and training and support feel disingenuous. This runs counter to the NIOSH Total Worker Health® approach, which recognizes rest, recovery, and supportive organizational policies as core prevention strategies that reduce risk before harm occurs.1 It is time to apply the same prevention mindset to mental health that has long guided effective safety programs.
Mental Health Is Not Just Illness or Crisis – We all have it
Suicide rates in construction, mining, and other high-risk industries have rightly drawn national attention. These statistics are alarming and deserve sustained action. However, they do not tell the whole story.
For every highly visible crisis, there are many more employees experiencing chronic stress, anxiety, depression, sleep disruption, or substance misuse. These struggles often remain unseen, yet they affect concentration, decision-making, reaction time, and overall safety performance long before a crisis occurs.
Acknowledging that we all have mental health just as we all have physical health is a step towards reducing stigma and normalizing talking about mental health in and out of the workplace. Evidence-based trainings like Mental Health First Aid are very comprehensive at addressing everything from early warning signs to crisis intervention. MHFA includes cultural differences and understanding, how to encourage appropriate support and professional help, and role-playing scenarios for deeper learning.
Mental Health Near Misses: Early Warning Signs
In safety, near misses are treated as gifts: early signals that something in the system needs attention. Mental health has near misses, but they are easier to overlook.
Examples include:
- Increased irritability, conflict, or withdrawal
- Presenteeism—being physically present but disengaged or exhausted
- Frequent minor illnesses or increased absenteeism
- Changes in sleep, mood, or reliability
- Increased substance use or risk-taking
When these patterns are normalized as “just part of the job,” organizations lose the opportunity for prevention. Addressing mental health near misses is not about diagnosing individuals; it is about examining conditions and systems that may be contributing to strain. In isolation, one or two changes or red flags may be normal (example: lack of sleep due to a new baby or stress associated with an important deadline); however, it’s important to check in with someone as if these warning signs are prolonged or compounded. They are an indicator that a full-blown illness or crisis may be looming.
The Business Case: Direct Costs Employers Can’t Ignore
The National Safety Council’s Mental Health Employer Cost Calculator2 translates mental health risk into clear, employer-relevant cost data, something safety professionals can act on. This is a tremendous resource if you need some concrete data to build your advocacy for mental health awareness trainings or other mental health investments.
Here is an example of the cost calculator in action (you can plug in your own company’s state, industry, and size): For a 350-person construction company in Arizona, the estimated annual cost of employee mental distress exceeds $400,000.
These costs are driven primarily by:
-
- Lost work time and reduced productivity
- Employee turnover and retraining
- Health care utilization and expenses
These impacts affect staffing stability, fatigue levels, error rates, and the conditions under which incidents are more likely to occur.
The calculator report highlights an important prevention opportunity: while mental distress carries significant costs, investments in mental health support consistently deliver returns. Research cited by NSC shows that for every $1 invested in mental health support and treatment, employers realize an average $4 return through reduced absenteeism, improved productivity, and lower turnover. From a safety perspective, this underscores the value of intervening upstream, when corrective action is most effective and least costly.
Culture Is an Upstream Control Measure
Safety professionals are familiar with the hierarchy of controls. While engineering and elimination controls often receive the most attention, administrative and cultural controls play a critical role, especially in mental health prevention.
Upstream mental health solutions are less about awareness posters and more about how work is designed and supported day to day. A few examples of policy measures that you may want to explore deeper and choose one or two to prioritize include:
Paid Time Off – Policies that allow employees to take time away without fear of punishment or stigma reduce cumulative stress and support recovery. If we value prevention and encourage our employees to be seen by a medical professional for preventive check-ups including for mental health, they need to be in paid status to do so or else it is unlikely to happen. When taking leave is discouraged or unpaid then fatigue, burnout, and errors increase. A culture that values rest and routine preventive care ultimately supports safer performance.
Flexibility That Acknowledges Reality – Rigid schedules increase stress without improving outcomes. Thoughtful flexibility such as shift adjustments and predictable scheduling (knowing when one will be working daily, weekly and monthly) can significantly reduce strain at work and outside of work. Flexibility is not about lowering expectations. It is about recognizing that employees perform best when systems account for real human needs like family, hobbies, and planned time off.
Human-Centered Communication – Leaders do not need to be clinicians to support prevention. Consistent check-ins, noticing changes, and listening without judgment can surface concerns before they escalate. 92% of employees think that it is important to work for an organization that provides support for employee mental health. 95% report it’s important for the organization to respect boundaries between work and nonwork time.3 Formal and peer leaders can model good behavior by checking in regularly, being vulnerable with one’s own health and mental health goals, and maintaining privacy and confidentiality.
Safety Pros Cannot Carry This Alone
Worksite mental health is a shared responsibility. Safety professionals play a vital role, but they cannot carry the full focus of this company-wide effort any more than they can single-handedly control production pressures or staffing decisions.
Effective upstream prevention requires collaboration with:
-
- Human Resources, to align leave, benefits, and accommodation policies with well-being
- Operations and Leadership, to set realistic expectations and model healthy behaviors
- Occupational Health, EAPs, and Benefits Partners, to ensure timely access to support and promote positive aspects of all of these benefits
- Training and Learning Teams, to deliver evidence-based education that builds confidence and skills
When these functions operate in silos, prevention efforts stall. When they work together, mental health becomes part of the organization’s overall safety system.
Applying a Safety Lens to Mental Health
Safety professionals already have the tools needed to support mental health prevention:
-
- Identifying risk factors
- Understanding systems and root causes
- Valuing prevention over reaction
- Encouraging reporting and learning
- Building cultures where speaking up prevents harm
Applying these principles to mental health does not require reinventing the profession. It requires expanding the definition of what prevention includes.
Moving Upstream: A Call to Action
Mental health crises rarely occur without warning. The signals are often present—just unnoticed or unsupported.
Safety leaders can move upstream by:
-
- Treating mental health indicators as legitimate near misses
- Advocating for policies that reduce cumulative stress
- Partnering across departments to address root causes
- Reinforcing cultures of care, acceptance, and communication
Prevention has always been the heart of safety. By applying that same mindset upstream to mental health, organizations can reduce risk, improve performance, and protect workers—long before the fish begin floating downstream.
Resources
1 NIOSH Total Worker Health ® Program – NIOSH Total Worker Health® Program | TWH | CDC
2 National Safety Council Mental Health Employer Cost Calculator – https://www.nsc.org/workplace/safety-topics/employee-mental-health/cost-calculator
3 American Psychological Association – Work in AmericaTM Survey – 2023 – 2023 Work in America Survey: Workplaces as engines of psychological health and well-being


